Ovarian vein incompetence (leaky valve) is an under-recognised cause of pelvic pain and congestion in women, particularly those who have had children. Incompetence and reversed flow in the ovarian veins can also result in varicose veins on the vulva. Ovarian vein incompetence may also contribute to venous problems in the legs, such as recurrent varicose veins and leg pain related to the menstrual cycle.
Definition
Ovarian veins are designed to return blood from the pelvis back up to the heart. Antegrade flow towards the heart is augmented by a valve at the top end of each vein. Valvular dysfunction or incompetence causes reversed flow into the pelvis and results in internal venous varicocities. Pregnancy and the growing foetus may put pressure on the ovarian veins, causing dilatation and dysfunction of these valves. These dilated veins persist after delivery.
Cause
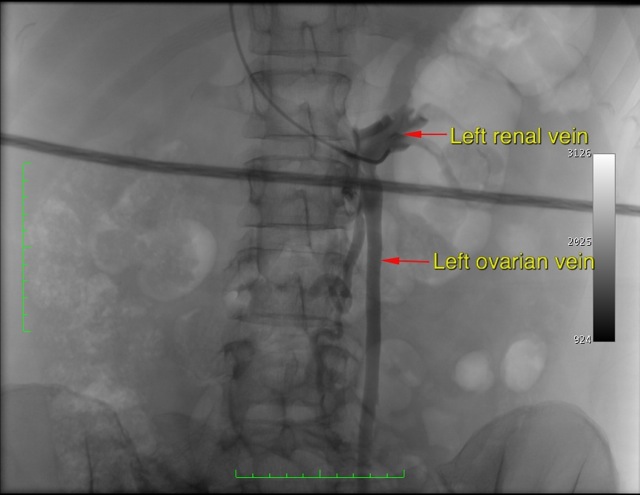
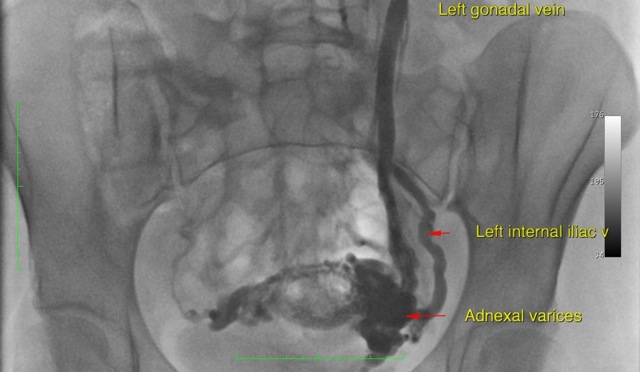
The blood from the left ovary drains up to the left kidney vein via the left ovarian vein. The right ovarian vein more commonly drains into the inferior vena cava (the large vessel draining the blood from the abdomen and legs) rather than the kidney vein. The junction of the left ovarian vein and the left kidney vein can cause problems if the valve in the vein does not work. If this valve is absent or does not work then blood from the left kidney will flow back from the kidney and into the pelvis causing a bunch of enlarged pelvic veins. This can cause varicose veins in the vulva and contribute to varicose veins in the leg. It can also cause the pelvic venous congestion syndrome.
There are non-invasive methods of diagnosing ovarian venous incompetence. A diameter of greater than 8mm measured on ultrasound or CT is diagnostic.
Symptoms arising from dilated ovarian varices include nagging pelvic or loin pain. This may be worse at the end of the day, after exercise or on prolonged standing. It may also cause urogential symptoms such as bladder irritation, menstrual pain and pain related to intercourse.
The condition is often under-recognised because these veins are internal. However in some cases, if the reflux is severe, the venous incompetence may manifest as varicose veins on the vulva, or worsening/recurrent varicose veins in the leg. In these cases, the ovarian vein needs to be treated adequately before the treating varicose veins in the leg.
Treatment
Embolization is a method of percutaneously occluding blood vessels. This is performed with a small catheter or tube, which measures less than 2mm in diameter. The entry point is a vein above the collar bone or the top of the leg. Both approaches are safe and equally comfortable. As no cut is made in the skin, no mark will be left on the skin. The catheter/tube is then navigated internally to the ovarian vein, within the pelvis. The veins are then occluded with small platinum or stainless steel coils. These mechanically obstruct the veins, causing them to clot and involute. Often, a sclerosant foam is also injected in order to reduce chances of the vein re-opening after the procedure.
A majority of cases involve treatment of the left vein only. Right sided varices can be caused by reflux across the midline from an incompetent left vein. In the unusual circumstance that both veins require treatment, these should be done in separate episodes in order to minimise post-operative discomfort.
Update - Since January 2015 Dr Steinfort has been treating this condition via an upper right arm incision. The incision point is still only 2mm, and the approach by the arm is even more comfortable, and less conspicuous.

Where does the blood go?
The refluxing ovarian vein does not contribute to venous drainage. The ovary would have developed longstanding "collateral" (alternate) venous drainage pathways. Coiling the ovarian vein should decrease the pressure on the ovary.
How effective is embolization?
The success rate for curing the incompetent vein is above 90% for embolization.
What happens after the procedure?
The procedure is normally performed under conscious ("twilight") sedation. After the a short period of recovery from sedation in the hospital, patients normally return home on the same day. Patients should not drive themselves home.
During the recuperation phase at home, the patient should remain well hydrated. Normal activity can be resumed the following day, but one should refrain from heavy lifting or prolonged exercise for several weeks. There may be some mild discomfort in the flank and pelvis in the following week. The following menstrual cycle may also be uncomfortable as there is some re-adjustment of the flow dynamics.
Afterwards, follow up with a phlebologist or vascular surgeon should be performed if you suffer from varicose veins in the legs. These will still require treatment but hopefully the outcome will be more permanent when the "leak" from the ovarian system is treated.
Are there any complications with embolization?
Minor complications may occur such as neck discomfort at the entry site, mild back ache and nausea. All of these symptoms normally resolve within a week. Migration of coils in the lungs is exceptionally rare and usually has no significant consequence.
Who are Interventional Radiologists?
They are doctors sub specialized in using minimally invasive techniques to treat disease using cutting edge technology and imaging guidance such as low-dose Xray, CT and ultrasound. In contradistinction to traditional surgery, there is no open surgical incision. As a result, hospital stay and recuperation times are much reduced and well tolerated.
Other Links
Other useful information ccan be found at the following link:
Society of Interventional Radiology - Chronic Pelvic Pain
CIRSE - Cardiovascular and Interventional Radiological Society of Europe


